
The platform helps you keep up with medical records with the assistance of built-in SOAP notes templates.
Soap notes software#
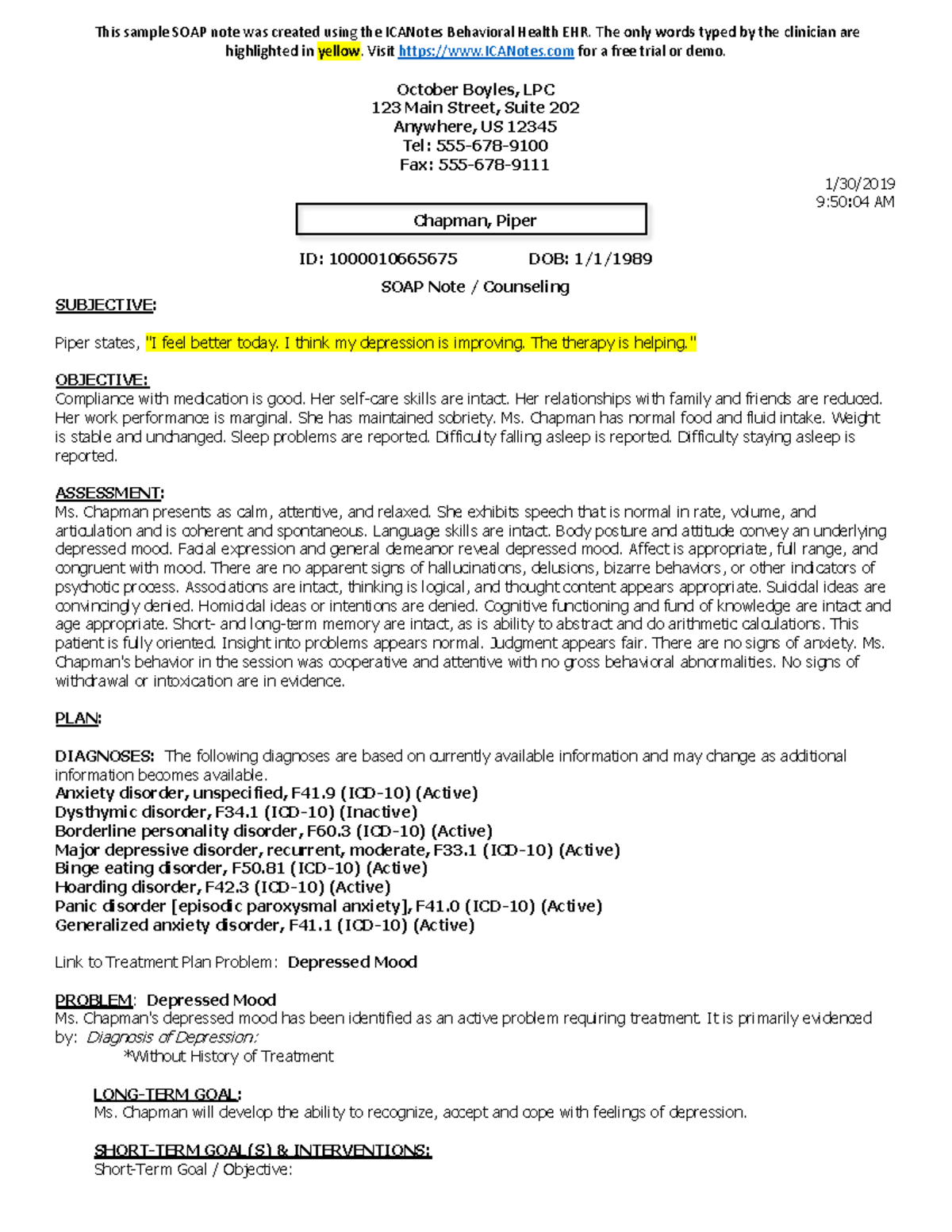
75Healthħ5Health is cloud-based electronic health record software for medical practices of any size. Read our complete product selection methodology here. These products are selected from Capterra’s electronic medical records software directory and listed alphabetically. We’ve listed the top three software tools that have SOAP note templates. With built-in SOAP notes, all patient records you enter are directly linked to and saved to your medical software. If you’re willing to invest, there are specific medical software systems that offer built-in templates.
Soap notes pdf#
The templates are available as PDF files and the size starts from 14KB.
Soap notes free#
Safety Culture: This website offers free SOAP notes templates for pediatrics and nursing.The formats for downloading the templates are DOC and PDF and the file size starts from 8KB. SampleTemplates: This website offers free SOAP notes templates related to nursing, physical therapy, pediatric, massage, clinical progress, and more.The templates are available in PDF format and the file size starts from 15KB. Template Archive: This website offers over 30 free SOAP notes templates for medical specialties including psychiatry, asthma, psoriasis, pediatric, and orthopedic.These templates are fully editable so you can easily make changes to them. Template Archive, SampleTemplates, and Safety Culture are three websites that offer free SOAP notes templates. The plan may even include details on the patient’s self-care, such as bed rest, days off work, and healthcare and lifestyle recommendations.Ī sample SOAP note used in a dental practice ( Source ) It may involve more tests to either confirm or rule out a diagnosis. It includes the treatment plan (e.g., medication, therapies, surgeries) you’ll follow for the patient. The last component of a SOAP note is the plan. There may also be cases where a definitive diagnosis is not made by the physician, therefore many possible diagnoses are included in the assessment.

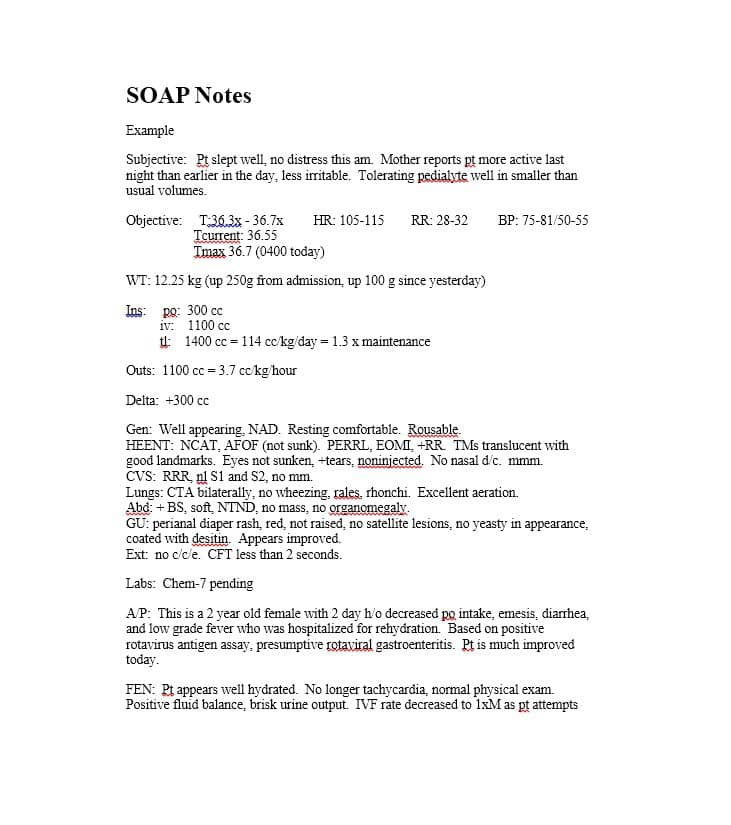
For any patient, there may be one clear diagnosis or multiple issues that require separate diagnoses. It includes a summary of your diagnosis of the patient’s existing condition. The next component of a SOAP note is assessment. You can also include details of previous diagnostics tests (e.g., X-rays) and lab reports.
Soap notes skin#
It has details of any visible symptoms such as changed skin color or any abnormalities you feel when physically examining the patient. It includes observations that can be measured such as body temperature, pulse rate, and blood pressure.

This is a record of your physical examination of the patient’s condition. Any comments, concerns, or questions your patients may have are also included here. Record your patient’s chief complaint, existing symptoms, and any pain description in this section. Notes from your verbal interaction with patients as well as what they tell you about their condition go here. This covers your patient’s detailed medical history and current symptoms. Since both use the same documentation method, there’ll be no miscommunication regarding a patient’s treatment plan or health status. They don’t have to go through the entire form to find the one tiny bit of information they require.Ī standardized SOAP note template also makes it easier to share records with other healthcare providers, if required. Each piece of information is entered into a specific field on the template, so medical providers know where exactly to find the information they need.
Soap notes manual#
All SOAP notes have a standardized format that is divided into four categories (which we’ll go over in the next section).īy organizing patient records in a defined template, these notes help cut down manual errors and miscommunication. Medical software tools with built-in SOAP notes templatesĪ subjective, objective, assessment, and plan (SOAP) note is a common documentation method used by healthcare providers to capture and record patient information, from the intake form and diagnosis to the treatment plan and progress notes.


 0 kommentar(er)
0 kommentar(er)
